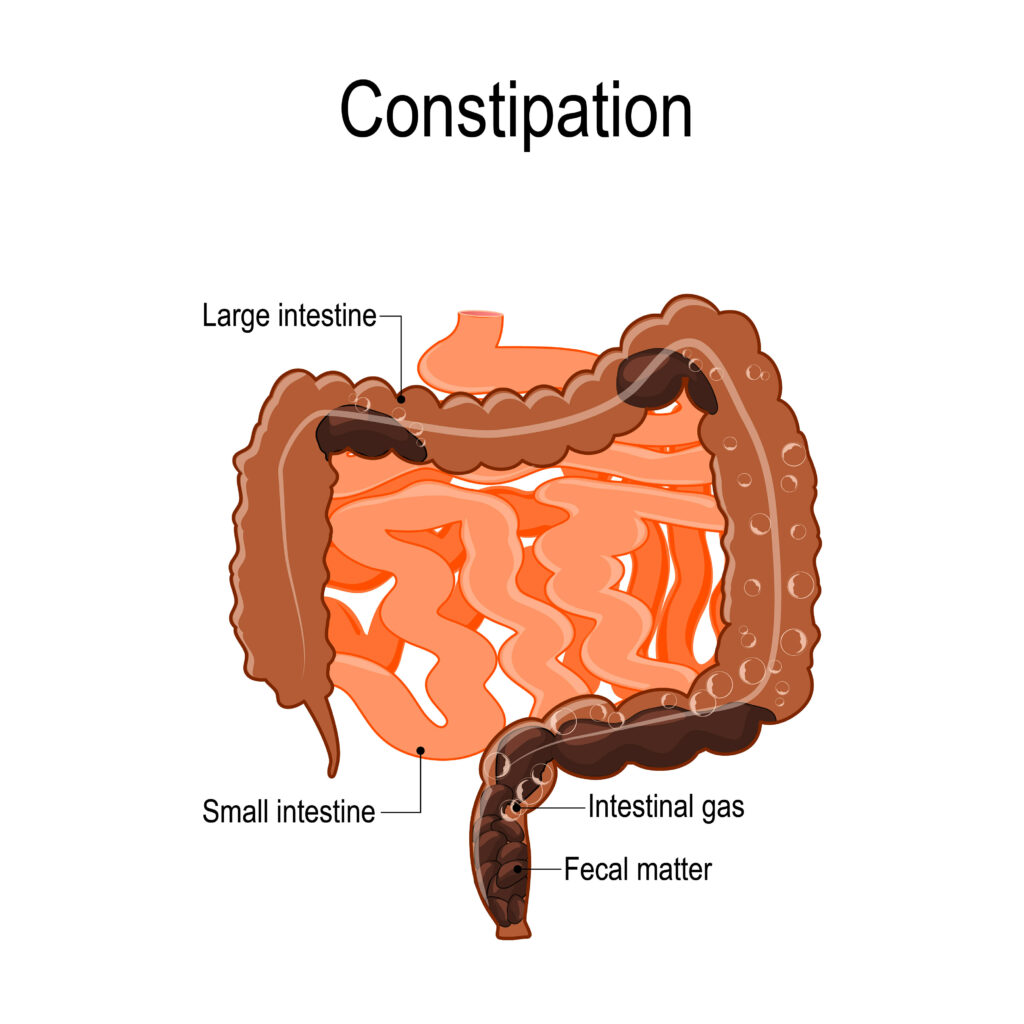
Chronic constipation means infrequent or difficult intestinal transit that persists for several weeks or more. In general, constipation is described as the situation of elimination of intestinal contents with a frequency of less than 3 stools per week. Although occasional constipation is very common, some people experience chronic constipation that interferes with their ability to carry out their daily activities. Chronic constipation can also cause excessive straining to pass stool. Treatment for chronic constipation depends in part on the pre-existing cause. However, in some cases, the cause remains undiscovered.
Blockages in the colon or rectum
Problems with the pelvic muscles involved in intestinal transit can cause chronic constipation
Diseases that influence the hormones in the body
Symptoms
Signs and symptoms of chronic constipation include:
- Under 3 chairs per week
- Hard seats
- Straining to defecate
- The sensation of blockage in the rectum that prevents intestinal transit
- The sensation of incomplete evacuation from the rectum
- Needing to help empty the rectum, such as using the hands to press on the abdomen or using the finger to remove feces from the rectum
Constipation can be considered chronic if you have experienced one or more of these symptoms in the last three months.
When to go to the doctor
Make an appointment with the gastroenterologist if you experience unexplained and persistent changes in the intestinal transit.
Causes
Constipation occurs most frequently when waste or feces pass through the digestive tract with difficulty or cannot be effectively eliminated from the rectum, which causes the stool to become hard and dry. Chronic constipation has many possible causes.
Blockages in the colon or rectum
Blockages in the colon or rectum can slow down or stop the movement of feces. The causes can be:
- Small trauma to the skin around the anus (anal fissure)
- A blockage in the intestines (intestinal obstruction)
- Colon cancer
- Narrowing of the colon (intestinal stricture)
- Other types of abdominal cancer that press on the colon
- Rectal cancer
- The rectum that presses behind the wall of the vagina (rectocele)
- Problems of the nerves in the colon and rectum
Neurological problems that affect the nerves cause the muscles of the colon and rectum to contract and move feces into the intestine.
The causes can be:
- Damage to the nerves that control body functions (autonomic neuropathy)
- Multiple sclerosis
- Parkinson’s disease
- Spinal trauma
- Stroke
- Difficulty in the muscles involved in the elimination of faeces
Problems with the pelvic muscles involved in intestinal transit can cause chronic constipation.
These problems can be:
- Inability to relax pelvic muscles to allow bowel movement (anismus)
- Pelvic muscles that do not properly coordinate relaxation and contractions (dysynergy)
- Weakening of the pelvic floor muscles
Diseases that influence the hormones in the body
Hormones help balance fluids in the body. Diseases and conditions that disturb the hormonal balance can cause constipation. These can be:
- Diabetes
- Overactive parathyroid gland (hyperparathyroidism)
- Pregnancy
- Underactive thyroid (hypothyroidism)
Risk factors
The factors that can increase the risk of chronic constipation are:
- Age
- Female
- Dehydration
- A diet low in fiber
- Lack of movement or sedentarism
- Certain medications, such as sedatives, opioid pain medications, some antidepressants or antihypertensives
- A mental condition such as depression or an eating disorder
Complications
Complications of chronic constipation can be:
- Inflammation of the veins at the level of the anus (hemorrhoids). Straining to have a bowel movement can cause inflammation of the veins around the anus.
- Trauma to the skin of the anus (anal fissure). Hard and large feces can cause minor trauma to the anus.
- Faeces that cannot be eliminated (faecal impaction). Chronic constipation can cause the accumulation of hardened feces that remain trapped in the intestines.
- Intestine coming out of the anus (rectal prolapse). Straining to have a bowel movement can cause a small part of the rectum to stretch and protrude from the anus.
Prevention
The following can help you avoid the development of chronic constipation:
- Include in your diet many foods rich in fiber, such as legumes, vegetables, fruits, whole grains
- Consume in small quantities foods with low fiber content, such as processed foods, dairy, and meat
- Drink plenty of fluids
- Stay as active as you can and try to exercise regularly
- Try to manage the stress
- Do not ignore the need to go to the toilet
- Try to create a regular schedule for going to the bathroom, especially after a meal
- Make sure that when the child transitions to solid food, he gets enough fiber from his diet
Diagnostic
In addition to the clinical examination and the digital rectal examination, the doctor can recommend the following analyses and investigations to diagnose chronic constipation and establish its cause:
- Blood Tests. The doctor will look for signs of a systemic condition such as hypothyroidism or high calcium levels.
- X-ray. An x-ray will help the doctor determine if the intestines are blocked and if there is feces present along the colon.
- Examination of the rectum, sigmoid colon, or lower colon. During this procedure, the doctor will insert a flexible tube with a light end into the anus to examine the rectum and the last part of the colon.
- Examination of the rectum and the entire colon (colonoscopy). This diagnostic procedure allows the doctor to visualize the entire colon with the help of the colonoscope – a flexible tube equipped with a mini-video camera at the end.
- Evaluation of the anal sphincter muscle (anorectal manometry). In this procedure, the doctor inserts a narrow and flexible tube into the anus, then inflates a small balloon located at the end of the tube. The instrument is subsequently removed through the sphincter muscle. The procedure allows the doctor to measure the coordination of the muscles you use for intestinal peristaltic movements.
- Evaluation of the speed of the anal sphincter (balloon expulsion test). It is sometimes used together with anorectal manometry; the procedure measures the time in which you expel the balloon filled with water and place in the rectum.
- Evaluation of how the food bowl passes through the colon (colonic transit study). During this procedure, you will swallow a capsule that contains either a radiopaque marker or a wireless recording device. The passage of the capsule through the colon will be recorded for a period of 24-48 hours and will be visible on the X-ray. In some cases, you can swallow a food activated with radiocarbon, and a special camera will record its passage (scintigraphy). The doctor will observe the signs of intestinal muscle dysfunction and the way the food bowl crosses the colon.
- Radiography of the rectum during defecation (defecography). During this procedure, the doctor will insert a soft barium paste into the rectum. Afterward, you will eliminate it during defecation. Barium appears on radiographs and can highlight a prolapse or problems with muscle function and muscle coordination.
- MRI defecography. In this procedure, as in barium defecography, the doctor will insert a contrast gel into the rectum. The MRI machine can visualize and evaluate the function of the muscles involved in defecation. This investigation can also diagnose the problems that cause constipation, such as rectocele or rectal prolapse.
Treatment
Treatment for chronic constipation usually begins with diet and lifestyle changes aimed at increasing the speed with which the food bowl passes through the intestines. If these changes do not help, the doctor can recommend drugs or surgery.
Changes in diet and lifestyle
Your doctor may recommend the following changes to relieve constipation:
- Increasing fiber intake. Adding fiber to the diet increases the weight of the stool and speeds up its passage through the intestines. Gradually start eating more fresh fruits and vegetables every day. Choose whole grains.
- The doctor can recommend a specific amount of fiber to consume daily. In general, try to get 14 grams of fiber for every 1,000 calories. A sudden increase in the amount of fiber can cause bloating and gas, so start slowly and add gradually over several weeks.
- Exercise most days of the week. Physical activity increases muscle activity in the intestines. Try to include physical exercise on most days of the week. If you are not already doing them, ask your doctor if you are healthy enough to start an exercise program.
- Don’t ignore the need to go to the bathroom. Do not rush, take enough time in the bathroom to solve the problem.
- Laxatives. There are certain types of laxatives. Each of them acts differently.
- Other medicines. If OTCs do not help you with chronic constipation, your doctor may recommend prescription drugs, especially if you have irritable bowel syndrome.
- Pelvic muscle training. Relaxation of the pelvic floor muscles facilitates intestinal transit.
- Surgery may be an option if you have tried other treatments and chronic constipation is caused by a blockage, rectocele or stricture.
In the case of people who have tried other treatments without success and who have abnormally slow intestinal transit, the surgical removal of a portion of the colon may prove to be an option. Surgery to remove the entire colon is rarely necessary.