Oral candidiasis is one of the most common conditions of the oral cavity and is caused by infection of the oral mucosa with various species of fungi, in particular Candida albicans.
What is oral candidiasis?
Oral candidiasis is one of the most common conditions of the oral cavity and is caused by infection of the oral mucosa with various species of fungi, especially Candida albicans.
Candida is a fungus normally found both in the integument and in the various mucous membranes of the body (oral, vaginal, intestinal). The pathogen causes infections through uncontrolled multiplication in people with a weakened immune system or those with imbalances of the saprophytic flora due to metabolic causes or after taking antibiotics (antibiotics selectively destroy the saprophytic flora and can favor the multiplication of yeasts).
The body’s immune defense mechanisms against oral candidiasis involve the recognition of yeast by host receptors located on the surface of epithelial cells of the oral cavity, secretion of antimicrobial peptides and proinflammatory factors represented by cytokines and chemokines with a signaling role and recruitment of phagocytes, neutrophils, macrophages and dendritic cells to the site of infection. Integrity of the oral mucosa, immune defense mechanisms and adequate salivary secretion are the main factors involved in the prevention of candida infections in the oral cavity.
The host immune system is an essential element that prevents candidiasis via T helper 17 cells involved in the defense mechanisms against infections with different Candida species. These lymphocytes control the growth of yeast in the lining of the oral cavity while inhibiting the pathogen’s ability to invade the yeast.
Why oral candidiasis occurs
Candida albicans is the main etiological agent involved in the occurrence of oral candidiasis and is responsible for about 95% of all cases of oral candidiasis. C.albicans is found in the commensal flora of the oral cavity, with 80% of the population having a healthy carrier status of this yeast. In addition to the mucosa of the oral cavity, Candida physiologically colonizes the gastrointestinal and reproductive tracts of healthy individuals, without generating specific local pathologies.
Candida is a versatile commensal pathogen that can easily adapt to changes in the body’s microbiota, with the ability to actively proliferate under certain favorable conditions. The virulence of the pathogen involved in the occurrence of oral candidiasis is due to the enzymatic equipment of the yeast, represented by surface adhesins, proteolytic enzymes (degrading cells generated in the body’s immune response) and those that determine the emergence of multidrug resistance of candida to different types of antifungal agents.
In the oral cavity, the co-adhesion of candida species with other bacteria that are part of the normal flora (Streptococcus mitis, S.gordonii, S.mutans, S.oralis readily adhere to candida hyphae and provide them with carbonic resources for growth and development), is among the main pathological mechanisms involved in the processes of over-colonization of the oral mucosa.
The main factors that favor the appearance of oral candidiasis are represented by:
- Poor oral hygiene especially in denture wearers
- Wearing of incorrectly finished prosthetic dental appliances that favor traumatization of the tissues of the oral cavity (jugal mucosa, gums, tongue)
- Smoking favors the development of oral candidiasis by decreasing the salivary flow and the pH of the oral cavity
- Antibiotics and inhaled or topical corticosteroids (gels applied to the oral cavity to treat certain lesions)
- Immune deficiencies in the elderly and young children (during the first months of life, infants have an underdeveloped immune system)
- Severe immune deficiency in HIV-positive patients, Jobs syndrome, Sjogren’s syndrome, graft versus host disease (in patients who have undergone heterologous transplantation) and those undergoing immunosuppressive treatments. In patients diagnosed with HIV, oral candidiasis is more commonly caused by C.dubliniensis, the severity of clinical manifestations being directly correlated with CD4 cell deficiency. In addition, this category of patients has low levels of antimicrobial peptide-histamine-5 compared to healthy individuals. Linear gingival erythema manifested as an erythematous line (red mucosa) at the free edge of the gums is specific to oral candidiasis in HIV-positive individuals
- endocrine imbalances: diabetes mellitus, Addison’s disease, hypothyroidism; diabetes mellitus favors the development of candida infections in the mouth through increased serum glucose concentrations
- Chemotherapy and radiotherapy, especially to the head and neck
- Nutritional deficiencies of iron, zinc, magnesium, selenium, folic acid, vitamin A, B6, B12 and vitamin C
- Pregnancy
What are the symptoms of oral candidiasis

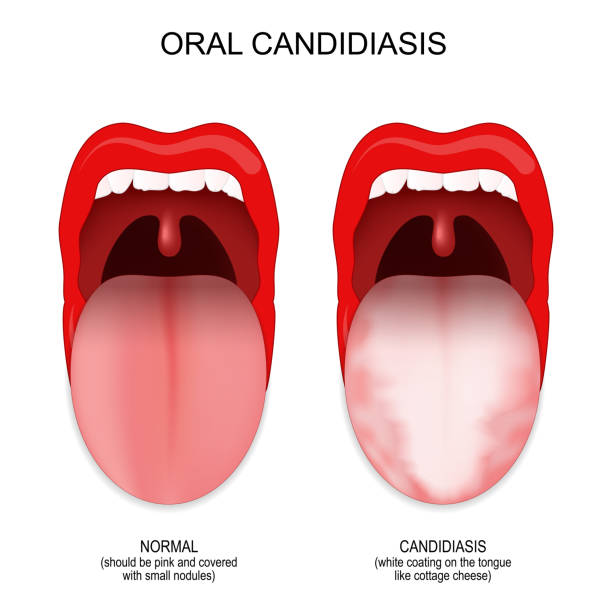
Oral candidiasis is an opportunistic infection with different Candida species that manifests itself by the appearance of whitish deposits (white spots) on the tongue and oral mucosa due to fungal overgrowth in the superficial tissues. The main reservoir of candida in the oral cavity is located in the posterior region of the tongue, from where the pathogen can spread to the oropharynx and oral cavity. Clinically, oral candidiasis can be acute or chronic, depending on the time period of the patient’s symptomatology.
Acute pseudomembranous oral candidiasis is manifested by the appearance of multifocal deposits with the appearance of whitish membranes on the tongue and oral mucosa or erythematous, which involves the appearance of erythematous lesions and is favored by antibiotic treatments (antibiotics selectively destroy the saprophytic flora and favor the multiplication of candida).
Chronic oral infections due to candida described in specialized literature include:
- atrophic oral candidiasis of the erythematous type is more frequently found in people with a deficient immune status due to infection with the human immunodeficiency virus, denture wearers and in individuals with inadequate oral hygiene
- angular cheilitis: this type of oral fungal infection affects the commissures of the oral cavity (corners of the mouth) and is manifested by erythema, maceration, cracks and crusts that generate increased discomfort for the patient
- cheilocandidosis manifested on the lips, involves the formation of ulcers and crusts on the lips and is frequently due to the use of pacifiers (in infants) and cosmetic products based on petrolatum
- leukoplakia occurs more frequently in the retrocommissural area (anterior oral mucosa) and the lateral parts of the tongue, especially in heavy smokers; this type of chronic oral candidiasis presents an increased risk of malignancy with the appearance of squamous cell carcinoma
- median rhomboid glossitis or atrophic glossitis manifests itself in the form of elliptical or rhomboid-shaped atrophy located at the base of the tongue and is due to smoking and the prolonged use of inhaled corticosteroids
- chronic mucocutaneous candidiasis syndrome represents an association of clinical manifestations that include the integumentary surface, nails, genital and oral mucosa, due to fungal infections, more frequently encountered in patients suffering from immunodebilitating pathologies: HIV, autoimmune ectodermal dystrophy
The specific symptoms of oral candidiasis are generally represented by:
- Burning sensation in the oral cavity and pharynx (esophageal candidiasis)
- The presence of whitish deposits adhering to the mucosa of the tongue, cheeks and gums
- Erythema of the oral mucosa
- Pain at the level of the lesions
- Bleeding of the oral mucosa during tooth brushing
- The presence of a persistent unpleasant taste
- Alteration of the sense of taste
- Oral candidiasis in infants and young children can cause the child to have difficulty feeding at the breast (the child sucks and swallows with difficulty due to the erythematous lesions caused by candida), irritability and weight loss. Oral candidiasis of the child is favored by natural birth if the mother has vaginal candidiasis, breastfeeding the child without following hygiene rules or using incorrectly sterilized teats and bottles
Diagnosis of oral candidiasis
The diagnosis of oral candidiasis is established by the otolaryngologist specialist based on the clinical examination of the patient and the paraclinical investigations represented by the culture of the lingual scraping, the bacteriological examination of the sputum or the pharyngeal exudate.
Treatment of oral candidiasis
The treatment of oral candidiasis is carried out according to the sensitivity of the isolated germ to various antifungals tested in the antifungigram. The method of administration of the antifungal medication depends on the severity of the infection and can vary from local administration of the treatment to systemic administration (oral administration), especially in the case of recurrent candidiasis or those extended to the esophageal, pulmonary or systemic level.
Reducing the risk of oral candidiasis can be achieved by applying a set of measures that include:
- adopting a healthy and balanced diet avoiding excessive consumption of sugars
- compliance with oral hygiene rules: brushing teeth 2 times a day, using mouthwash after brushing and interdental floss; correct hygiene of dental prostheses and mouthpieces; sanitizing oral inhalers
- the appropriate treatment of the conditions that favor the dryness of the oral mucosa – Sjogren’s syndrome and of the metabolic imbalances that cause the appearance of immune deficits – diabetes mellitus
- proper hygiene of the nipple before putting the infant to the breast; sanitizing teats and milk containers used by infants
Learn more:
- Oral candidosis – https://www.magonlinelibrary.com/doi/abs/10.12968/denu.2001.28.3.132
- Oral candidosis – https://www.cidjournal.com/article/S0738-081X(00)00145-0/fulltext
- Oral candidosis – http://www.quintpub.com/userhome/qi/qi_33_7_sherman_7.pdf